Non-invasive prenatal testing (NIPT) has become an important part of early pregnancy care, giving parents insight into their baby’s chromosomes through a simple blood test. But even if NIPT has been done, the 13 week ultrasound is still essential. For parents, it offers a first real look at how the baby is physically developing: seeing the heartbeat, movements, and early features that blood tests alone can’t show. For clinicians, this scan provides anatomical and placental information that NIPT cannot detect, such as structural abnormalities, growth patterns, and chorionicity in multiple pregnancies. Together, NIPT and ultrasound form a more complete picture, combining genetic information with visible evidence of development and maternal health.
In this fact sheet, we will explore:
- What NIPT Does and Doesn’t Do
- Key Assessments at 13 Weeks
- Detecting Early Concerns
- Screening for Maternal Health
- How Results Shape Care
—————
1. What NIPT Does and Doesn’t Do
NIPT is a powerful tool, but it has limits. For parents, it’s helpful to know what questions a blood test can answer — and what still requires an ultrasound. For clinicians, understanding the complementary role of each test ensures a balanced approach to screening.
What NIPT does well:
- Detects common chromosomal conditions such as Trisomy 21 (Down syndrome), Trisomy 18, and Trisomy 13
- Can also check for sex chromosome conditions (depending on the test type)
- Provides a high degree of accuracy, reducing the need for some invasive tests
- Uses a simple blood sample, posing no risk to the pregnancy
What NIPT doesn’t do:
- Does not check the baby’s anatomy or detect structural abnormalities
- Cannot show how the placenta is forming or functioning
- Cannot confirm growth, heartbeat, or the number of babies
- May still require follow-up ultrasound or diagnostic testing if results are high risk
| NIPT | 13 Week Ultrasound |
|---|---|
| Analyses cell-free placental DNA in maternal blood | Provides a real-time view of the baby and placenta |
| Detects chromosomal abnormalities with high sensitivity and specificity | Detects structural abnormalities (brain, face, spine, heart, limbs, abdomen and abdominal wall) |
| Non-invasive to the pregnancy, no physical risk to the developing fetus | Non-invasive, visual reassurance for parents |
| Cannot assess physical growth or maternal health risks | Screens for preeclampsia risk and placental development |
| Often done from 10 weeks onwards | Performed between 13 weeks and 13 weeks 6 days |
In practice, NIPT answers questions about chromosomes, while the 13 week ultrasound answers questions about development and health.
2. Key Assessments at 13 Weeks
During the 13 week ultrasound, several important checks are carried out to build a clear picture of how the pregnancy is progressing. The scan confirms the baby’s heartbeat and viability, providing reassurance while also establishing cardiac activity, rhythm, and rate. Growth is measured through the crown–rump length, which is the most accurate way to confirm gestational age and due date between 11 and 14 weeks.
The scan may also determine the number of babies, if not confirmed during an early dating/viability scan, confirming whether it is a single or multiple pregnancy. In multiple pregnancies, chorionicity and amnionicity are identified, which are essential for planning care. Placental development is reviewed, with the location and attachment site documented so any early concerns can be monitored.
Finally, an early anatomy review is performed, allowing a first assessment of the brain, face, heart, spine, abdomen, abdominal wall, limbs, and other structures. While detailed anatomy scans follow later in pregnancy, this early survey can sometimes detect major abnormalities, giving families and clinicians valuable information sooner.
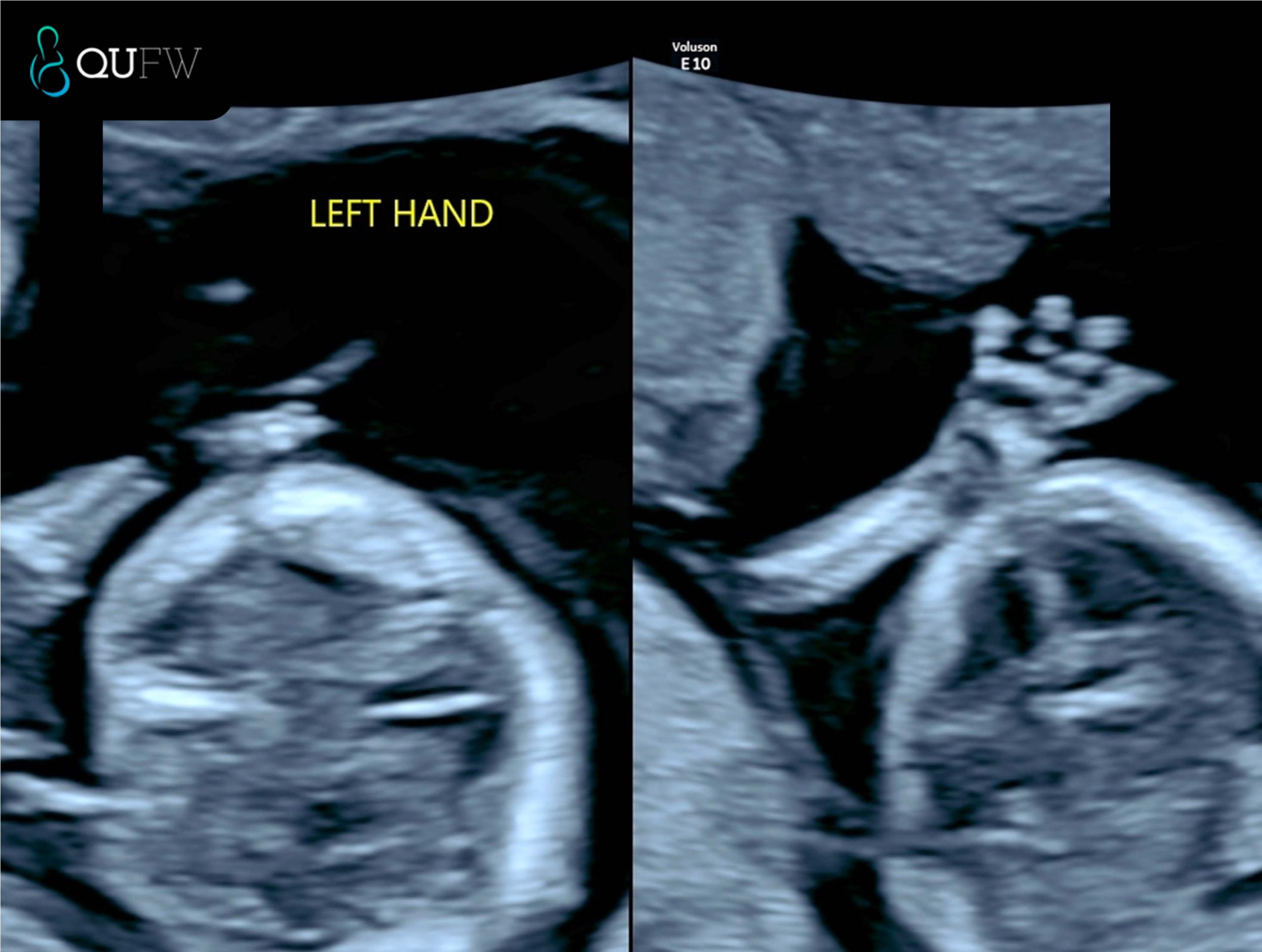
Early structural assessment of the upper limbs
3. Detecting Early Concerns
One of the main strengths of the 13 week ultrasound is its ability to highlight potential issues earlier in pregnancy, giving families more time to understand their options and clinicians more time to plan care.
Areas where concerns may be detected include:
- Structural abnormalities such as issues with the brain, face, spine, abdomen, abdominal wall, or limbs
- Chromosomal indicators like increased nuchal translucency or absent nasal bone
- Placental concerns that could affect growth and development later in pregnancy
- Signs of complications in multiple pregnancies, such as unequal sharing of the placenta
| Possible Concern | What the Scan May Show | Next Steps |
|---|---|---|
| Brain or skull abnormality | Absence of skull bones (acrania), irregular brain structure | Referral for detailed scan, genetic counselling |
| Facial structures | Absence of the Nasal bone, suggestion of early features of cleft lip/palate, facial development of the orbits | Referral for detailed scan, genetic counselling |
| Spinal abnormality | Abnormal curvature, incomplete closure of spine | Specialist ultrasound, ongoing monitoring |
| Abdominal structures | Presence of stomach, diaphragm, bladder, kidneys, 3 vessel cord | |
| Abdominal wall defect | Organs seen outside abdominal cavity as in exomphalos, gastroschisis | Referral to tertiary care, surgical planning |
| Increased NT or absent nasal bone | Higher chance of chromosomal condition
Further assessment of fetal cardiac structures |
Follow-up with NIPT, CVS, or amniocentesis
Further cardiac evaluation in the event that the NT measures >3.5mm and low risk NIPT or normal karyotype has been performed. |
| Placental issues | Abnormal attachment such as early detection of Placenta Accreta Spectrum. | Monitoring, follow-up scans later in pregnancy |
| Twin complications | Discordant growth, shared placenta risks | Closer surveillance, specialist input |
By identifying these concerns early, the 13 week scan helps guide whether further investigations or specialist referrals are needed. It is not a diagnosis on its own but an important first step in recognising when closer attention may be required.

Early structural assessment of the spine
4. Screening for Maternal Health
The 13 week ultrasound also provides information about the mother’s health and how the pregnancy may progress. A key focus at this stage is the risk of preeclampsia, a condition that can cause high blood pressure and complications later in pregnancy. The scan can be combined with maternal blood pressure readings, blood test results, and medical history to estimate the likelihood of developing preeclampsia. If a higher risk is identified, early interventions such as low-dose aspirin and closer monitoring can be recommended, improving outcomes for both mother and baby.
Placental development is another area of assessment. The position and quality of the placenta are reviewed to ensure it is developing normally and providing adequate support for the pregnancy. Identifying placental issues early helps clinicians plan follow-up care and keep a close watch on the baby’s growth throughout the second and third trimesters.
5. How Results Shape Care
The results of the 13 week ultrasound, especially when considered alongside NIPT, shape how care is managed for the rest of the pregnancy. Together, the two tests provide a comprehensive view: NIPT offers insight into the baby’s chromosomes, while ultrasound shows physical development, placental function, and maternal health factors. This combined approach helps guide decisions about further testing, the need for specialist referrals, and the level of monitoring required.
For parents, this means reassurance that the pregnancy is being tracked with the best tools available, and that potential issues can be identified earlier rather than later. For clinicians, it provides a structured baseline that supports personalised care throughout the pregnancy.
The 13 week ultrasound is therefore much more than a milestone moment to see the baby on screen. It is a pivotal point in early pregnancy care, one that combines emotional connection with medical precision. Used together with NIPT, it ensures families and healthcare providers have the clearest possible picture to support a safe and healthy journey ahead.
====================
Content Disclaimer
The information provided on this website is for educational and informational purposes only. It is not intended as a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your obstetric doctor or other qualified provider with any questions you may have regarding a medical condition or treatment and before undertaking a new healthcare regimen.
The content on this website is not intended to be a comprehensive source of information on any particular topic and should not be relied upon as such. The authors and publishers of this website are not liable for any damages or injury resulting from the use or misuse of the information provided on this website.


0 Comments