The 13 week ultrasound is one of the most important early scans in pregnancy. Usually performed between 13 weeks and 13 weeks 6 days, it gives parents a first detailed look at their baby’s growth and development, often providing reassurance as they see the heartbeat, movements, and forming features. At the same time, this scan holds significant clinical value. It marks the end of the first trimester, when crown–rump length measurement is most accurate for dating the pregnancy, nuchal translucency assessment is most reliable, and an early structural survey can detect major anomalies. These combined insights make the 13 week ultrasound both a meaningful milestone for parents and a cornerstone of first trimester screening and early pregnancy care.
This fact sheet covers these topics:
- Why the 13 Week Scan Matters
- Early Anatomy Check
- Chromosomal Abnormality Screening
- Maternal Health Screening
—————
1. Why the 13 Week Ultrasound Matters
The 13 week ultrasound plays a key role in checking that your pregnancy is progressing as expected. It confirms your baby’s heartbeat, measures growth, and if not confirmed in an earlier viability ultrasound can identify whether you are carrying one baby or multiples. Its major purpose is to assess the early anatomical structures that have developed by 13 weeks. The scan can also assess the placenta to check its position is appropriate at this early gestation, however it is important to note that placental position is largely checked at the 20 week morphology assessment. For parents, these checks bring reassurance that things are on track, while for clinicians, they provide vital data for guiding care for the ongoing pregnancy.
At this stage, crown–rump length measurement helps establish accurate gestational age, chorionicity can be determined in multiple pregnancies, and the position of the placenta is documented. Together, these findings set the foundation for monitoring both maternal and fetal health as the pregnancy continues.
2. Early Anatomy Check
At around 13 weeks, ultrasound technology allows a first look at your baby’s developing anatomy. For parents, this is often the first time you see just how much detail has already formed, including tiny hands and feet, the curve of the spine, and the outline of the brain. For clinicians, this scan provides a systematic review of early structures that can reveal major anomalies at an earlier stage than later pregnancy scans.
Key areas assessed include:
- Brain, skull and face – ensuring the skull is formed, the brain appears normal for this gestational age and the early facial structures are developed
- Spine – checking alignment and early closure of the neural tube
- Heart – confirming rhythm and looking at the early chambers
- Abdomen and abdominal wall – ruling out major structures such as diaphragm, stomach, kidneys, bladder and abdominal wall defects
- Limbs – confirming presence and movement of arms and legs
| What parents see | What clinicians assess |
|---|---|
| Baby’s profile, head, and movements | Cranial structure, early detection of acrania or anencephaly, early brain development and evidence of early signs of Open Neural Tube Defects (ONTD’s)
Early facial structures and early detection of facial clefts. |
| Curved spine on screen | Spinal alignment and signs of neural tube defects |
| Tiny heartbeat flicker | Cardiac rhythm, chamber development |
| Wriggling arms and legs | Limb formation, detection of limb reduction anomalies |
| Abdomen outline | Integrity of the abdominal wall, exclusion of exomphalos or gastroschisis |
| Abdomen | Abdominal structures such as the diaphragm, stomach filling, presence of both kidneys, appropriate bladder filling, evidence of 3 vessel cord and cord insertion. |
For parents, these images are a reassuring sign of normal growth. For clinicians, they provide a vital opportunity to detect significant problems early, allowing for referral to specialist care if required.
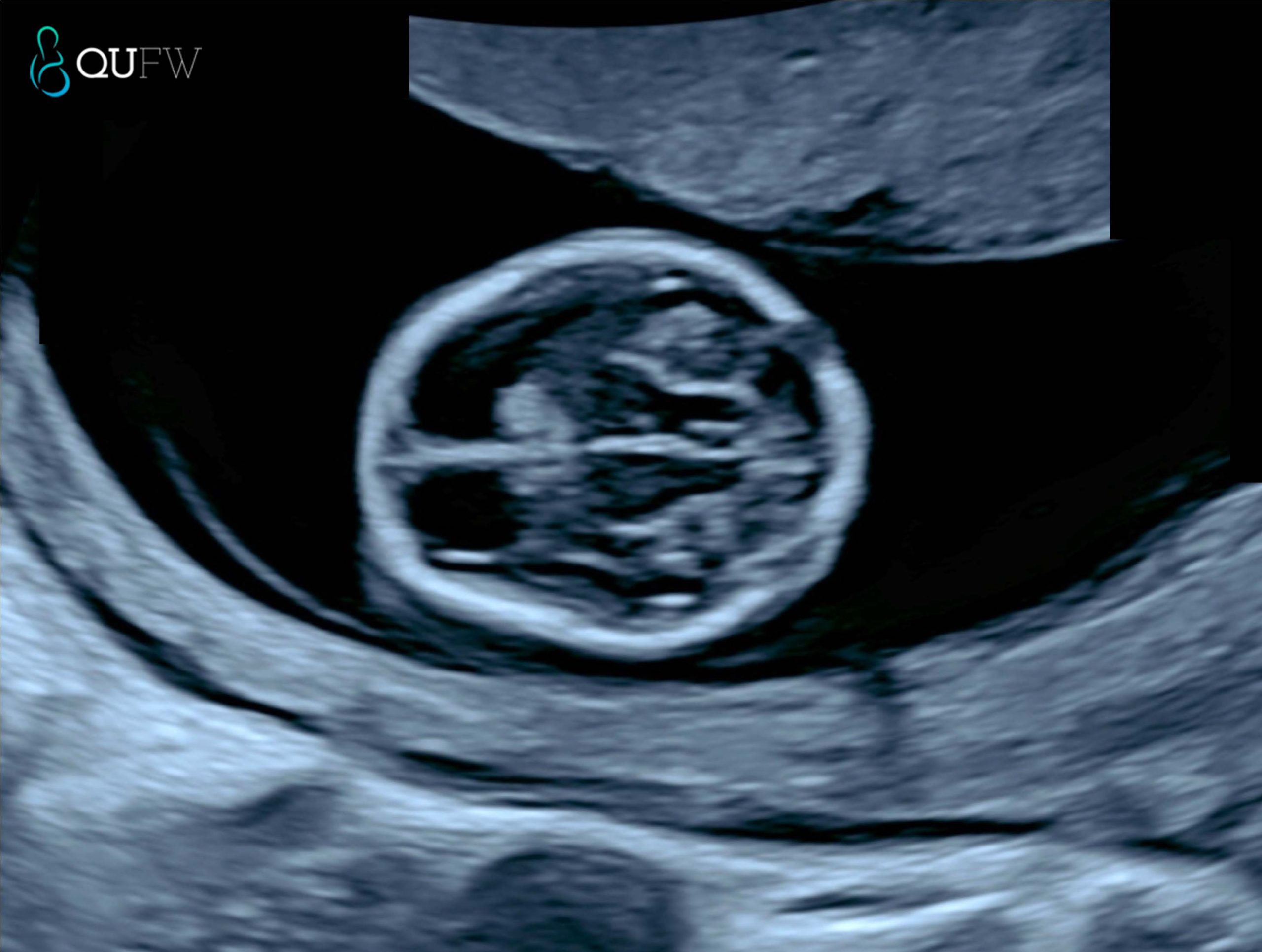
Early structural assessment of the fetal brain
3. First Trimester Combined Screening – Chromosomal Abnormality Screening
The 13 week ultrasound can also help assess the risk of chromosomal conditions, such as Down syndrome (Trisomy 21), Trisomy 18, and Trisomy 13.
In the absence of NIPT screening, a First Trimester Combined Screening (FTCS) may be performed to provide a risk assessment screening for Trisomy 21, Trisomy 18 and Trisomy 13 by utilising the risk assessment algorithm provided by the Fetal Medicine Foundation. An early anatomy assessment scan is performed at the same time as the FTCS assessment.
In the event that a NIPT screening has been performed, it has been recommended by ISUOG International Society of Ultrasound in Obstetrics and Gynaecology under the consensus statement that “First-trimester risk estimates for trisomies 21, 18 and 13 based on nuchal translucency measurements and maternal biochemistry should not be computed in a woman who has already received a normal NIPT result for these trisomies” (reference here).
The Fetal Medicine Foundation (FMF) algorithm is a first-trimester prenatal screening method for Trisomy 21 (Down Syndrome) that uses maternal age, fetal nuchal translucency (NT) ultrasound measurements, and maternal serum markers (free beta-hCG and PAPP-A) to calculate a risk score. The algorithm helps identify pregnancies at higher risk for Trisomy 21, but it’s a screening tool, not a diagnostic test, and a higher risk score may lead to further invasive tests like amniocentesis or chorionic villus sampling (CVS).
How the FMF Algorithm Works
- Maternal Age: Maternal age is a fundamental factor, as the risk of Down Syndrome increases with maternal age.
- Ultrasound (NT Measurement): A detailed first-trimester ultrasound is performed to measure the nuchal translucency (NT), a collection of fluid at the back of the fetus’s neck.
- Biochemical Markers: Maternal blood is tested for two hormones:
- Free beta-hCG (free beta-human chorionic gonadotropin): Typically elevated in Down Syndrome pregnancies.
- PAPP-A (pregnancy-associated plasma protein-A): Generally lower in Down Syndrome pregnancies.
- Risk Calculation: The FMF algorithm combines these factors to generate a personalised risk for Trisomy 21, Trisomy 18 and Trisomy 13.
For parents, this part of the scan offers important reassurance or an early signal that further testing may be needed. For clinicians, it provides measurable markers that contribute to first-trimester combined screening.
Markers typically assessed at this stage include:
- Nuchal translucency (NT): a fluid space at the back of the baby’s neck that, if increased, can indicate a higher chance of chromosomal abnormality.
- Nasal bone: its presence or absence can be a significant marker in risk assessment.
- Ductus venosus flow: abnormal flow patterns may be associated with aneuploidy or cardiac defects.
- Tricuspid regurgitation: when present, it can increase the risk profile.
| For parents | For clinicians |
|---|---|
| The scan looks at small features, like the fluid behind the baby’s neck and nose bone, that can indicate a higher or lower chance of conditions such as Down syndrome. | NT is measured between 11+0 and 13+6 weeks when CRL is 45–84 mm; when combined with maternal serum biochemistry (free β-hCG, PAPP-A), this forms the basis of first-trimester combined screening.
It is preferred at QUFW to perform this assessment between 13 weeks and 13+6 days |
| A higher-than-expected NT doesn’t mean something is wrong, but it may lead to follow-up testing for clarity particularly for congenital heart defects or other genetic syndromes. | Integration of ultrasound markers with serum and maternal age yields detection rates of >90% for Trisomy 21 at a 5% false-positive rate.
In the event of an NT measurement >3.5mm, further structural assessment of the fetus including the heart for congenital heart defects is made as part of the early anatomy scan. |
| Results can help guide whether additional tests, such as NIPT or diagnostic procedures (CVS, amniocentesis), are recommended. | Ancillary markers (nasal bone, ductus venosus, tricuspid regurgitation) improve specificity and refine risk stratification. |
In practice, this means the 13 week scan is more than just a “look at the baby” moment. It forms a crucial part of early screening that combines visual markers, blood tests, and clinical context to give the clearest picture possible at this stage of pregnancy.

Nuchal translucency assessment
4. Maternal Health Screening
The 13 week ultrasound is not only about checking the baby, it also provides valuable information about the mother’s health. For parents, this means doctors can look for early signs of conditions that could affect the pregnancy, helping to keep both mother and baby safe. For clinicians, this scan offers an opportunity to assess maternal risk factors and build a plan for ongoing care.
One of the key conditions that can be screened for is preeclampsia, a complication that can lead to high blood pressure and other serious health issues later in pregnancy. At this stage, the scan can be combined with blood pressure readings, maternal history, and blood test results to estimate a woman’s risk. If the risk is found to be higher, preventive steps can be started early.
The scan may also highlight placental concerns. Early assessment of how the placenta is developing and where it is attached provides important insight into how well it might support the pregnancy. These checks give reassurance to parents while helping clinicians take proactive measures if any issues are identified
====================
Content Disclaimer
The information provided on this website is for educational and informational purposes only. It is not intended as a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your obstetric doctor or other qualified provider with any questions you may have regarding a medical condition or treatment and before undertaking a new healthcare regimen.
The content on this website is not intended to be a comprehensive source of information on any particular topic and should not be relied upon as such. The authors and publishers of this website are not liable for any damages or injury resulting from the use or misuse of the information provided on this website.

0 Comments